The Reason Dental Screenings are Important at Any Age
February 21, 2019
Did you know that bad breath in your pet could be a sign of serious dental disease? February is National Pet Dental Health Month and to highlight the importance of routine, year-long, dental hygiene practices we have gathered a couple interesting stories from our patients at Care First.
Introducing: Farrah Pawcett

At eight months old, Farrah Pawcet came in for her first veterinary visit. Her mom reported that she had terrible breath and wouldn’t eat any hard food. Farrah wouldn’t allow her mom to open her mouth or touch her gums. All her adult teeth were present, so it was unlikely that this level of inflammation was caused by teething. She was diagnosed with severe gingivitis, which would best be solved with a professional dental cleaning procedure.
Farrah was scheduled for blood work, full mouth dental x-rays, and a deep cleaning under general anesthesia. At only 9 months of age, tooth resorption was evident on x-rays and the gum tissue was so fragile and diseased that it bled with gentle cleaning. After the procedure, the doctor recommended that Farrah’s mouth be rechecked in 4 weeks to determine if the inflammation had responded to the cleaning.
At Farrah’s recheck it was determined that she responded well to her post-operative care which consisted of antibiotics, anti-inflammatory medication, supplements for her immune system, and softened food; however, the gingivitis and bad breath persisted. In light of this information, she was diagnosed with an autoimmune condition called Gingivostomatitis. This condition caused her immune system to attack the enamel on her teeth and caused a painful inflammation of the gums. It is not fully known why some pets get this disease; however, purebred animals are more frequently diagnosed. The best treatment option for her condition was removal of the teeth.

Ginigival Inflammation 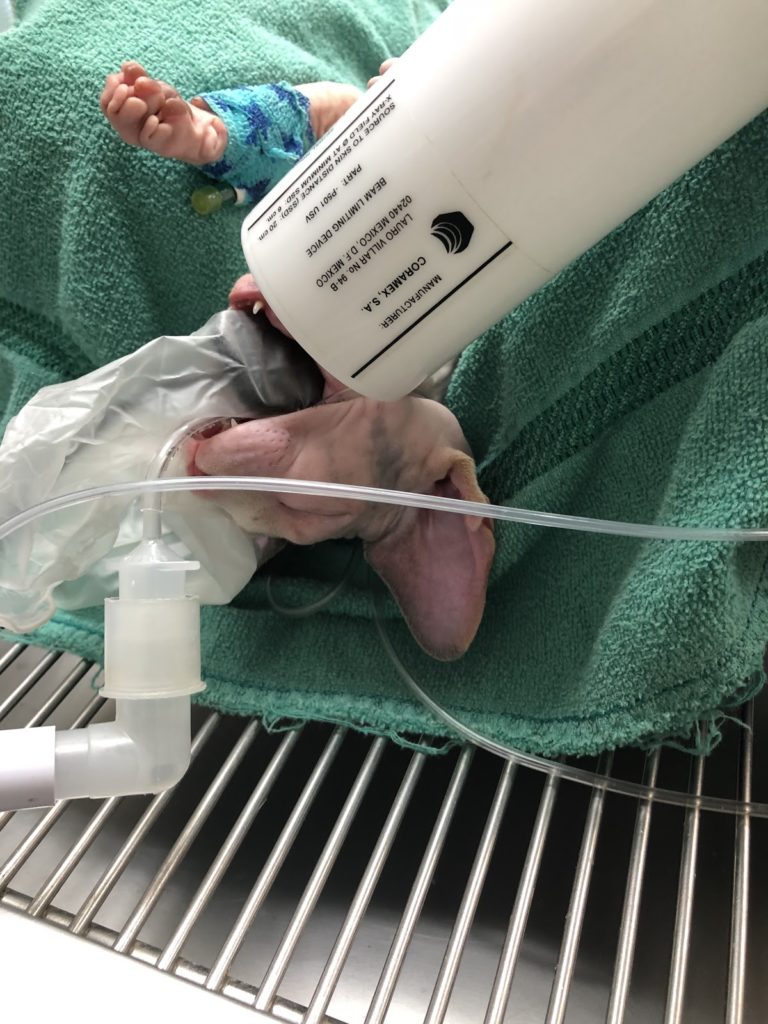
Farrah getting her x-rays
Farrah’s mom was uncomfortable with this difficult treatment plan. She worried about her quality of life, her facial expressions, her ability to do well under general anesthesia for a long period of time (especially since she has no fur!), the pain of recovery, and the overall cost. Since Farrah ate well and gave no indication of pain at home, her mom tried to manage the disease medically until she had saved enough money to consider surgery.
Farrah’s painful, inflamed gums and bad breath continued to persist despite all at home treaments. After addressing many of Farrah’s mom’s concerns, she finally decided she was ready for the big surgery because nothing else was working. Dr. McConnell prepped the surgical team the morning the morning of surgery, and Farrah arrived shortly after with anti-anxiety and pain medication in her system to prepare her for the big day.

X-Rays before extractions 
X-Rays after extractions
The surgical team ran a pre-anesthetic blood panel to ensure she was healthy enough to filter out anesthesia and began to warm her up while she was getting sleepy. Once she was under general anesthesia, full mouth dental x-rays were taken to identify any changes that would affect the surgical approach. Her diseased gums and all of her teeth were removed and post-operative dental x-rays were taken to make sure no tooth material was left.
Farrah did fantastic! Her oral surgery was successful and her pain control was excellent. She received multiple modes of pain control, including laser therapy on her gums after surgery. She was delivered into her mom’s arms at the end of the day and ate a whole can of cat food that night!
Her mouth will continue to be rechecked every two weeks to make sure the inflammation and bad breath resolves, and Farrah’s mom will continue to give her an Omega Fatty Acid supplement to support her immune system for the next 6-8 months. Farrah will now be able to have a long life without painful dental disease!
“Even though the thought of anesthesia is scary, and knowing your pet won’t have any teeth may make you feel some guilt, knowing your pet won’t have constant pain in their mouth outweighs these things. Farrah has been purring up a storm and acting 100% herself since surgery and I am so pleased with my decision and excited for her life to be pain free!”
Farrah’s Mom
Introducing: Basil

Basil is a much loved member of our hospital family and during his most recent exam an area of gum tissue overgrowth was identified. There was a strong odor coming from his mouth and the gingiva in this area had grown so large it almost blocked a tooth from view. As a Pug, Basil is a member of the Brachycephalic breeds of dogs which very commonly comes with an under bite. Under bites make oral home care and annual dental cleanings under general anesthesia really important
.
Basil had pre-anesthetic blood work and was scheduled for a comprehensive oral and radiographic assessment under general anesthesia.
Basil arrived for his procedure with his typical excitement upon seeing us! Once he was in a nice state of anesthesia, full mouth x-rays were taken. His dental x-rays identified two teeth that were rotated 90 degrees and putting pressure on the roots of the neighboring teeth. One of the rotated teeth (an incisor) was close to the root of the canine (the longest tooth in the mouth). It was important to remove these teeth because of the negative impact they were having on some of the more important teeth in the mouth, and they are very hard to brush!
After Basil’s x-rays were reviewed by the doctor, a thorough oral exam was done. He had some Buccal Granulomas from where he had chewed on the inside of his mouth. The gingival enlargement we saw in the room was present in multiple locations. Bacteria, hair, and plaque were stuck between the tooth and the abnormal gum tissue which caused the ligament that holds the tooth in its socket to become weakened and detach. In some cases, if this detachment is mild, a tooth can be preserved with deep scaling and an oral suture. If the detachment is too severe, the best option is to remove the tooth and clean out the socket. If the affected tooth is a “strategic tooth”, i.e. a tooth that is important for crunching (like some molars and premolars) or is a long or multi-rooted tooth (like the canines), then it may be worth visiting a board certified Veterinary Dentist for advanced treatment options.

Example of gingival enlargement similar to Basil’s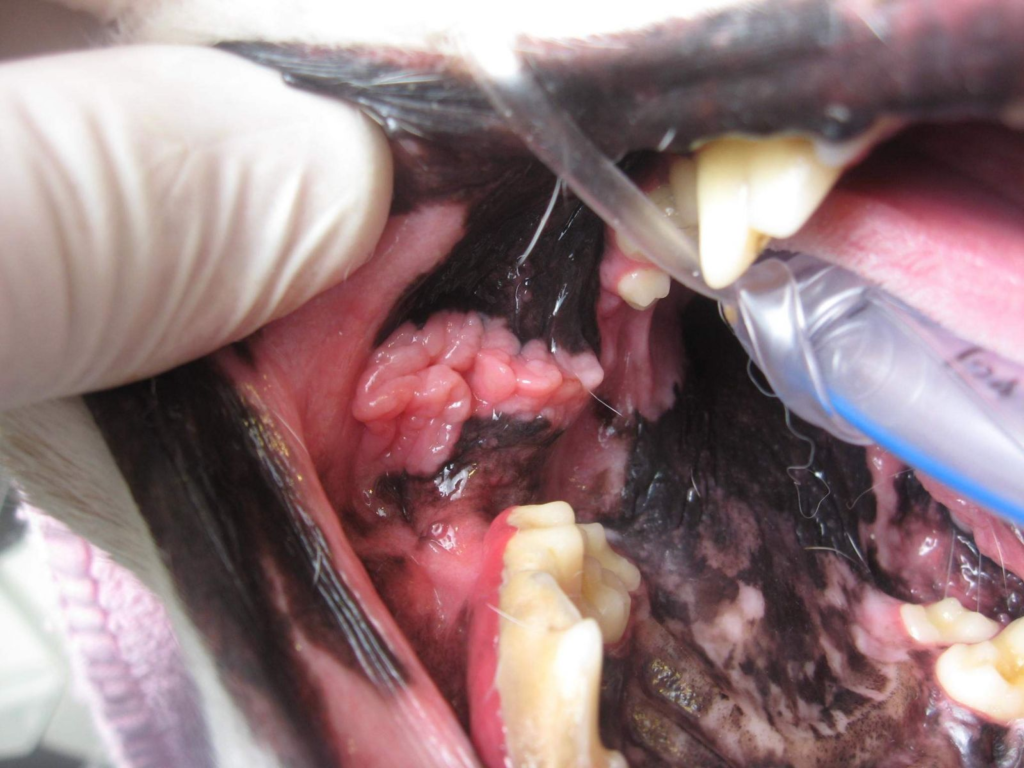
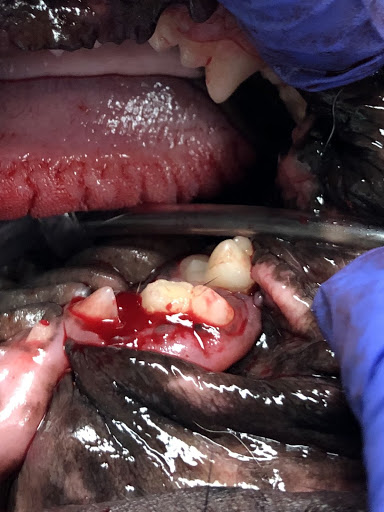
Example of Buccal Granuloma
Luckily, the teeth affected by gingival enlargement in Basil’s mouth were incisors which are not strategic teeth and removal doesn’t impact his quality of life. These non-strategic loose teeth were removed and the areas where the gingiva had overgrown were trimmed to allow Mom better access with her toothbrush.
There was a suspicious fracture in one of the largest premolars in the mouth – a major crunching tooth – which was evident on x-ray, oral exam, and probing. The affected tooth was the upper fourth premolar, a 3-rooted tooth that is very important for crunching kibble and hard treats. The fracture was very severe and cut across two of the 3 roots making a root canal impractical. Basil’s heart rate would increase a little bit with probing of this tooth so a nerve block was given and extraction of the tooth roots was performed. This same tooth on the other side was not fractured but some of the enamel had been chipped off.
What Did Basil Chew ON?
The rest of Basil’s teeth were scaled above and below the gums and polished smooth. Oral sutures were placed in his mouth to close the sockets and those will dissolve over the following weeks. He was given some extra pain medication since he had oral surgery and had a very smooth recovery.
Basil will go home with pain medication and instructions to eat a soft diet for 2 weeks until his recheck exam.
After speaking with Basil’s mom about his oral assessment and treatments, Mom recalled hearing a cracking sound several months prior when she gave Basil a bully stick. Ah ha!!!! While the gingival enlargement and rotated teeth are simply problems due to his genetics, the bully stick is something we can definitely eliminate to prevent problems in the future.
As a rule of thumb I always recommend oral toys and chews that are BENDABLE. If it doesn’t hurt if I whack you in the knee with the toy or treat, then it’s safe for the mouth.
For a list of chews that are also good for teeth you can visit www.vohc.org.
Back to Blog





